n healthcare advancement, ensuring that medical innovations address patients’ needs is paramount. Target Product Profiles (TPPs) are critical tools in product development, aligning regulatory requirements, market needs, and commercial objectives. However, a crucial voice is often missing: that of the patients themselves. By integrating direct insights from people with lived experience and expertise throughout the TPP development process, we aim to catalyze the creation of new diagnostics that directly respond to patient need.
Collaborating with patient advocacy groups offers a window into the diverse perspectives within a patient community, helping companies tailor development strategies to better meet the needs of those living with a condition. This commitment to co-creation is likely to lead to better outcomes for companies, reducing the risk of wasted effort and resources, as well as delivering products that genuinely resonate with their intended users.
While prioritizing patient involvement in developing TPPs may provide benefits, this process isn’t without challenges. It requires additional time, effort, and resources to ensure meaningful engagement, facilitate dialogue, and generate consensus views across diverse stakeholders, from people with lived experience to representatives from industry, the clinic, regulators, and payers.
For complex, chronic conditions like CF, this patient-centered approach to TPP development is invaluable. Recent advances in treatment have created new diagnostic challenges, making input from those with lived experience more crucial than ever. By involving people with CF in creating diagnostic TPPs from the outset, we aim to ensure that future innovations tackle the most pressing challenges faced by the community, ultimately improving patient care and quality of life.
The Urgent Need for New Diagnostics to Manage Infections in CF
CF is a life-limiting genetic condition that affects over 162,000 people across 94 countries. Caused by mutations in the CFTR gene, it leads to a buildup of thick, sticky mucus in the respiratory, digestive, and reproductive organs. In the lungs, this predisposes patients to frequent infections that are difficult to clear, causing exacerbations and a progressive decline in lung function.
People with CF routinely require antibiotics to manage chronic respiratory infections. However, treatment failure due to antimicrobial resistance (AMR) is increasingly common in this vulnerable population. While the discovery and development of new antimicrobials is an urgent unmet need, there are also limitations with current diagnostic approaches. These include a slow turnaround time for pathogen detection and a lack of clinical utility in existing antimicrobial susceptibility tests. These factors highlight the pressing need for accurate and reliable new diagnostic tools.
The introduction of highly effective CFTR modulators has significantly improved the lives of many people with CF by reducing mucus in the lungs and promoting airway hydration. However, this advancement has created an unexpected diagnostic challenge. Many patients can no longer produce on-demand sputum, which has been the primary sample for diagnosing lung infections. This issue, combined with pre-existing difficulties in obtaining sputum from children and some adults, highlights a critical need for innovation in diagnostic technologies, specifically, the development of new methods to effectively sample airways without relying on sputum.
The urgency of this need was reflected in the 2022 James Lind Alliance refresh of the priorities for research in CF, where the patient community ranked the diagnosis of lung infections in the absence of sputum as a top priority. This underscores the importance of evolving diagnostic technologies to keep pace with recent advances in standard care.
Working with the CF Community to Develop TPPs
The CF AMR Syndicate, jointly led by Medicines Discovery Catapult, Cystic Fibrosis Trust, and LifeArc, is a cross-sector initiative that brings together leading experts in CF and AMR from industry, academia, and clinical care, alongside people living with the condition, to accelerate the development of new CF antimicrobials and diagnostics.
In collaboration with the Newcastle NIHR HealthTech Research Centre, the CF Syndicate engaged more than 150 experts from across the sector and people with lived experience to develop a suite of patient-focused TPPs for CF lung infection and exacerbation diagnostics.
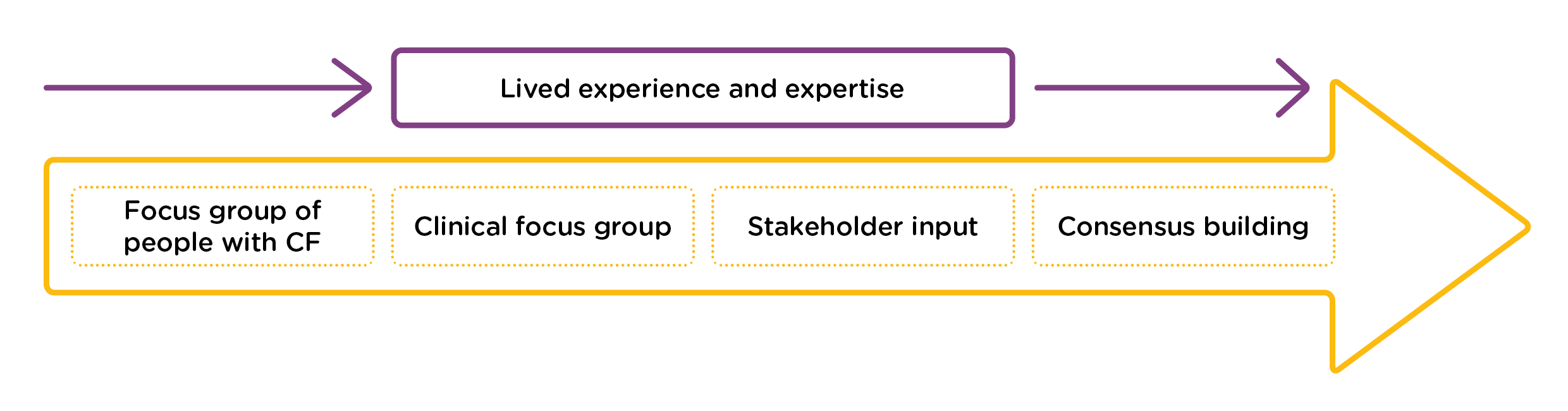
Our process unfolded in several key stages:
- Initial Review: Mapping diagnostic practices and tools, both in use and under development.
- Focus Group Consultation: Engaging people with CF, their families, and CF multidisciplinary care teams across the UK to define the unmet needs and practical considerations.
- Stakeholder Input: Incorporating additional perspectives, including those working in clinical microbiology laboratories and the diagnostic industry, to develop a suite of TPPs.
- Consensus Building: Surveying relevant stakeholders, followed by a virtual symposium to further refine the TPPs and discuss challenges and opportunities.
A Springboard for Innovation
These open-access TPPs provide a blueprint for innovators to focus diagnostic discovery efforts where they’re needed most. While developed in the UK, their intended impact is global, aiming to drive the creation of more effective and accessible diagnostic tools for the CF community worldwide. The CF AMR Syndicate is actively exploring options for accelerating the development of diagnostics aligned with the TPPs.
The CF community, including patients and their clinical care teams, possesses extensive knowledge and expertise. They are eager to collaborate with industry to incorporate their lived experience into the development of new medical innovations. This collaborative environment is supported by a very active global network of patient advocacy groups, specialist CF centers in the UK and other countries, extensive patient registries, and established clinical trial networks. Moreover, diagnostics developed for CF could potentially benefit people with other respiratory conditions, such as chronic obstructive pulmonary disease (COPD) and bronchiectasis.
This approach to TPP development could be considered a case study and applied to other disease indications and medical innovations. Innovators are encouraged to engage with people with lived experience to gain deeper insights into their needs. People with lived experience can provide valuable input on the acceptability and tolerance of new innovations, contributing to the development of more effective and patient-friendly products.
Acknowledgements:
Alison Halliday, Natasha Ratcliffe, and Members of the Diagnostic TPP project (Kile Green, Nicola Howe, Rachel Dakin, Raasti Naseem, Paula Sommer, Neill Gingles)

