TransCelerate BioPharma, Inc.
Novartis
CDISC
espite the stated intent to adopt digital technologies in the clinical development area of R&D, uptake has been relatively slow. There are various reasons for this, not the least of which is how we think about documenting critical regulatory required information. Despite significant technical advances in our ability to document (the verb) this information, we are stuck with documents (the noun) in a way that locks important data in paper or electronic forms of paper (docx, PDF, etc.), often camouflaged in unstructured blocks of text.
Of the many processes requiring manual curation, none is a better example of its limitations as part of study start up as setting up a database and electronic data collection tools. Again, data collection tools are generally configured as electronic forms of paper. This remains a pain point and delays the start of a clinical trial despite significant efforts to optimize processes. In fact, two separate surveys conducted by the Tufts Center for the Study of Drug Development in 2017 and 2020 show no improvement at all in cycle time metrics that capture the time between the protocol finalized to the database go-live date, which is estimated as greater than 65 business days or 13 weeks.
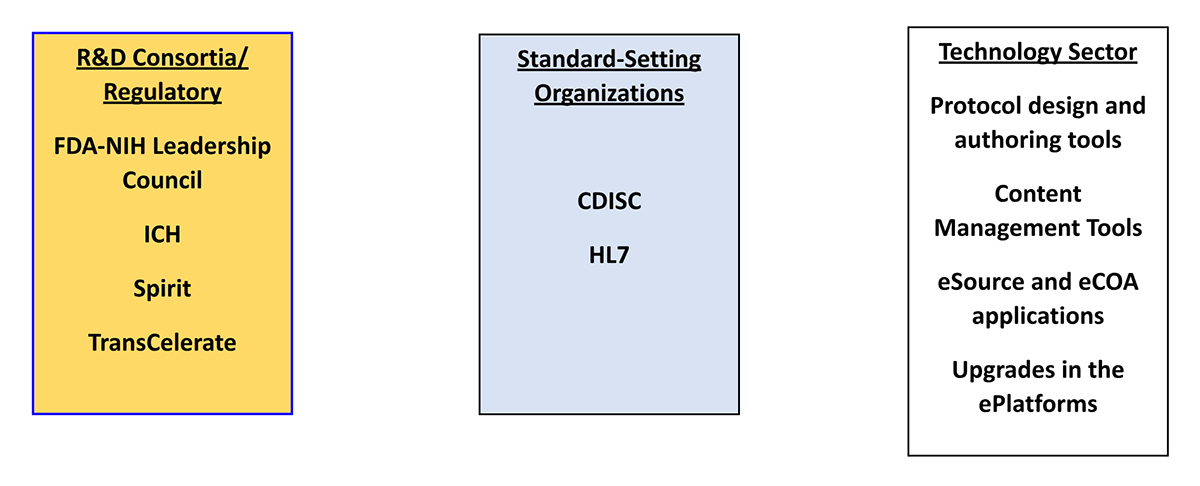
Globally, multiple organizations and sectors have been developing building blocks that may be considered foundational to the digital transformation of the end-to-end research process.
TransCelerate’s Common Protocol Template (CPT) shares many similarities with the published ICH guideline. Given its wide adoption across the industry and a wide variety of research organizations, this should make compliance more manageable than it was in the past when new guidelines were published. The CPT, informed by CDISC’s Clinical Data Standards effort, has already helped biopharmaceutical companies move away from company-specific protocol specifications that present challenges to investigator sites, ethics committees, regulatory reviewers, third-party collaborators, and other common stakeholders.
The ongoing collaboration between CDISC and TransCelerate using an open-source approach to develop a Unified Study Definitions Model (USDM) will issue its second release in July 2023. The USDM is delivered as a data model (i.e., names, attributes, cardinality, relationships) with controlled terminology definitions, an implementation guide, and a reference architecture with application programming interface (API) specifications. The scope of the USDM includes study definition information found in protocol documents such as general study information—phase, therapeutic area, indication—study design, schedule of activities and assessments, workflow and eligibility, and biomedical concepts to specify protocol-required data.
Along with the USDM, the creation of a Study Definitions Repository (SDR) establishes a backbone for documenting important protocol-specified information in a digital format and accelerates the implementation of its API-based exchange with a variety of platform systems and digital solutions that require it to execute a variety of clinical development functions including data capture, study planning, and operational functions. In addition, exchange with electronic medical record systems is enabled to automate site-based workflows and configuration of eSource data collection consistent with protocol requirements transmitted digitally in a machine-readable format. This fundamentally enables the “document once, read many times” concept.
On June 6, 2023, CDISC and Vulcan, an HL7 FHIR Accelerator, jointly announced their intention to utilize the USDM to accelerate the development of the content model envisioned as part of the ICH M11 project. This effort is supported by a Joint Leadership Forum that includes CDISC, ICH, TransCelerate, and the Vulcan Accelerator.
The real opportunity of this project is to bring together the collective know-how and the previously established building blocks. In the healthcare provider sector, which in essence represents the investigator sector, the patient experience has become increasingly digitized. The ability to harmonize and utilize existing standards for data exchange is becoming critical. As patient-facing applications used in clinical research proliferate, combined with the desire to bring research closer to patients through convergence with clinical care, the ability to leverage HL7 FHIR standards is equally as logical and critical to creating a digital bridge between clinical research and clinical care. This is a classic example of innovation through collaboration and a path to true digitalization of the clinical research protocol.
Assuming that the future state reflects successful convergence of clinical care and clinical research, it might be possible to envision:
- For the patient: Greater awareness of and access to clinical trials and an opportunity to contribute health data to answer research questions. A lower participation burden or friction could be recognized since data collected during routine care could be used to answer safety and efficacy questions along with providing information about relative effectiveness. Return of patient data could be more streamlined and efficient and available to their care provider earlier. Conceptually, research sponsors could bring studies to patients instead of trying to recruit patients into studies.
- For the sponsor and site: A broader site footprint that leverages the same clinical care infrastructure for both study conduct and data acquisition should reduce redundant procedures and data entry as well as the need to be facile with multiple data acquisition platforms. Connectivity between digital protocols and electronic health records enables automation for patient selection and workflows.
- For clinical research and care: Accelerating participant recruitment through the benefits above is aspirational, but just as important, the expanded awareness, access, and footprint should deliver better representativeness of patient participation. The ability to plug and play with emerging technology (best in breed) will not be limited by bespoke system integrations.
Today’s study-specific approaches to data exchange challenge all three stakeholders because of the time, effort, and cost of achieving it at the expense of being able to generate timely insights from that data.
The release of CeSHarP technical specs and the evolution of the USDM creates the opportunity for the industry to recognize that the benefit is tightly tied to both the pace and the means of implementation. It is important for implementers and end users to commit to using the published standards to take full advantage of the benefits of digital in study start up and abandon the burning platform of today’s document-driven, manual processes.

