Proceedings: DIA 2019 Global Annual Meeting

Keynote Address
DIA
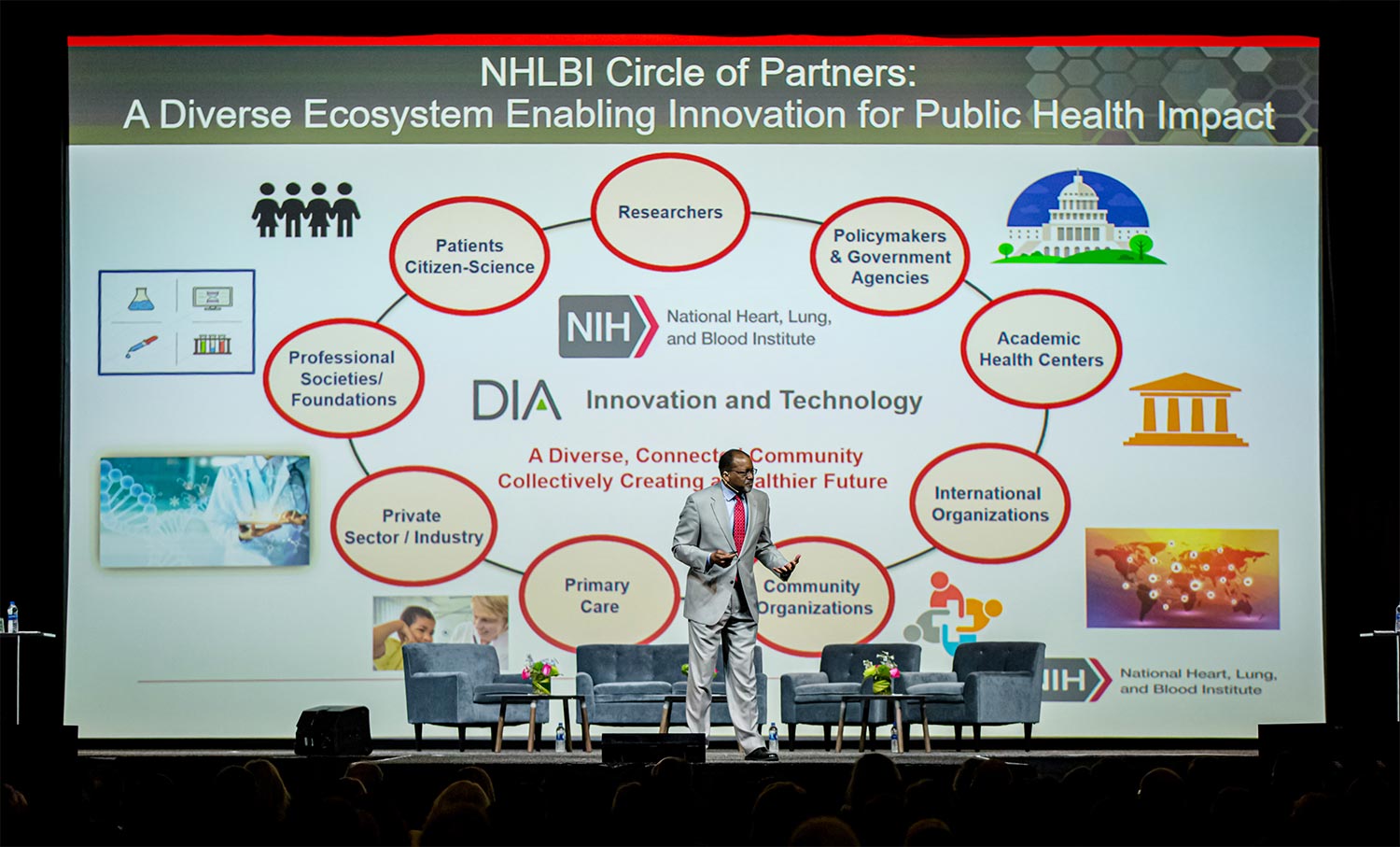
n today’s dynamic science and healthcare world, DIA 2019 provided an overarching reminder that patients are at the center of everything we do. In the keynote address given by Gary Gibbons, Director of of the National Heart, Lung, and Blood Institute (NHLBI), he stressed the importance of patients in the ecosystem of biomedical research. Over the course of an engaging 45-minute talk, Gibbons wove in his own history to drive home NHLBI’s mission of using translational and discovery science to enhance human health, and how the advancements of science have a significant public health impact.
Key Takeaways
- Collaboration drives innovation between basic science, industry, and implementation science, and encompasses the value of public-private partnerships.
- The social determinants of health and health inequities impact biopharmaceutical science and industry, and a systems approach to thinking about issues is key.
- Here’s a challenge: How do we drive innovation and scale our science to have a true global impact in reducing the burden of diseases?
Throughout his address, Gibbons demonstrated the importance of collaborations across scientific disciplines, and the cycle between observational studies, basic research, public health implementation science, clinical research, and the role of industry. At the beginning of the cycle, discovery science’s role in finding molecular targets to create effective interventions feeds into the importance of defining risks and benefits, informing evidence-based policies to drive implementation science, leading to a healthier population. At the core of this cycle is the patient, driving the need for scientific innovation and collaboration across federal partners, patient networks, academia, organizations, and industry.
From these points on the importance of a systems approach, Gary Gibbons segued into his own life story, starting with his grandmother’s roots as a sharecropper in Georgia. He spoke about her work ethic, the importance she placed on education, and most touchingly, how she “had a boldness of vision, to take a leap of faith” and move to a completely unfamiliar Philadelphia, to “create a better life for the next generation.” From this inspiring story, Gibbons moved on to tackle the issues of health inequities and disparities facing our world, and how part of creating a better life for the next generation is to reduce this gap.
The social determinants of health underwrite public health issues facing any community, and the idea that “ZIP code determines our health trajectory” leads into the need to apply a systems approach to solving these complex issues. While health disparities begin in the housing and social environment, or the “exposome,” they affect an individual and family’s access to a healthy lifestyle. For example, people living in a “food desert” area don’t have the same access to fresh produce and sources of nutrients. While there is still much to discover, we know enough about the human microbiome to know that proper nutrition is critical to a healthy gut and intestinal bacteria. Advances in science allow us to understand how environmental factors can influence the microbiome, the immune system, and the epigenome, and shed light on how gene/environment interactions play into health disparities.
With these social determinants of health, Gibbons emphasized the importance of adding value in the community and utilizing methods of community-based participatory research in addressing health issues. He cited the example of implementing blood pressure screening and medication adherence interventions at local barber shops, an important fixture in African-American communities. Through a nationwide rollout of this program, communities where this intervention was implemented saw lowered rates of high blood pressure. By engaging the community and building trust, we can achieve better health outcomes and decrease health disparities, he argued.
Gibbons closed with a reference to sickle cell disease, and where emerging technologies can be leveraged to facilitate global impact. As he spoke about the burden of this disease, the collaborations needed to think about novel gene therapies and emerging technologies, Gibbons challenged the crowd to think about the possibility of developing delivery systems that don’t require the same high-cost intensive care as immunotherapies of years past. He further urged the audience to envision the possibility of not only delivering effective gene therapies to cities such as Philadelphia and Detroit but also scaling this to reach high-burden areas in sub-Saharan Africa and around the world. By bridging science, public health, and his own story, Gibbons delivered an engaging message of how innovation and collaboration make better patient outcomes possible worldwide.

